If you want to use a third-party application (3rd Party App) that connects to Molina Healthcare to access your protected health information (“PHI”), please read this important information.
Molina Healthcare requires 3rd Party Apps to provide us written confirmation that they meet certain requirements when accessing Molina Healthcare member PHI. This is called an attestation. It also gives us confirmation that the 3rd Party App provider agrees to specific requirements to keep PHI confidential and secure. You can view this attestation by clicking on “Interoperability: Third-Party Application Registration Statement”.
If the
3rd Party App you want to use does not agree to our attestation or does not respond, we will notify you. You can change your mind about using the
3rd Party App to get your PHI from us. If you do not respond timely, letting us know if you’ve changed your mind, then we will share your PHI with the
3rd Party App, in accordance with applicable law. If the
3rd Party App is a risk to the security of Molina Healthcare’s information systems, we will not allow the
3rd Party App to connect to our systems and your PHI will not be shared with the
3 rd Party App. In order to protect your PHI, we recommend only using a
3rd Party App that has agreed to Molina Healthcare’s attestation.
Things to Consider when Choosing a 3rd Party App
It is important that you understand how a 3rd Party App uses and discloses your personal information, which may include PHI and other health information. It is also important that the 3rdParty App you choose keeps your personal information private and secure. Below are some tips on information to look for and ask when choosing a 3rd Party App.
- Do you understand how to use the 3rd Party App to access your personal information?
- Does the 3rd Party App require the use of passwords for you to access your personal information?
- Does the 3rd Party App have an easy-to-read Privacy Policy that clearly explains how the 3rd Party App will use and disclose your personal information? The Privacy Policy should explain how you will be informed of any changes to the policy. If the 3rd Party App does not have a Privacy Policy, we recommend that you choose a different 3rd Party App.
- What PHI and other personal information will the 3rd Party App collect? Will the 3rd Party App collect non-health information? Will the 3rd Party App collect other information from your mobile device, such as your location or information about your family and/or friends?
- How does the 3rd Party App store and use your personal information? Where does the 3rd Party App store your personal information? For example, will your personal information be stored in the United States or will it be transferred or accessed outside the United States?
- Does the 3rd Party App sell or share your personal information with third parties? If it does, the 3rd Party App’s Privacy Policy should explain why and to whom.
- Can you limit how the 3rd Party App uses and discloses your personal information?
- Does the 3rd Party App have reasonable and appropriate security measures to protect your personal information?
- Does the 3rd Party App have a clear and easy-to-understand process to handle user complaints?
- If you no longer want to use the 3rd Party App or if you no longer want the 3rd Party App to have access your to your PHI, is there a clear and easy process to terminate the 3rd Party App’s access to your PHI and other personal information?
- Does the 3rd Party App have a policy for deleting your PHI and other personal information once you terminate the 3rd Party App’s access?
Your health information is very sensitive information, and you should understand how 3rd Party Apps protect the privacy and security of your health information. We recommend that Molina Healthcare members only use 3rd Party Apps with strong privacy and security standards to protect individuals’ health information.
Your Privacy Rights
As a healthcare consumer, you have privacy rights that are protected under law. The federal law that gives you these protections is called the Health Insurance Portability and Accountability Act (HIPAA). The U.S. Department of Health and Human Services (HHS) Office for Civil Rights (OCR) enforces HIPAA. HIPAA generally applies to covered entities that include health plans and health care providers, and “business associates” that provide service to those plans and providers. You can find more information about HIPAA at:
To learn more about filing a complaint with OCR under HIPAA, please visit HHS Complaints.
It is important to understand that many 3rd Party Apps are not covered by HIPAA, particularly those that are offered directly to you as an individual, rather than through a health plan or provider. This means your health information will not be subject to the same privacy and security protections that health plans and providers must adhere to. 3rd Party Apps are regulated by the Federal Trade Commission (FTC) and the protections provided by the FTC Act; however, if the 3rd Party App is located outside the United States, the FTC may not able to fully protect your information. You can find more information from the FTC about mobile 3rd Party App privacy and security at FTC Mobile Apps. If you think a 3rd Party App has misused or violated your privacy, you can file a complaint with the FTC using the FTC complaint assistance at FTC Complaint Assistance.
Interoperability is an easy way to access and share your Health Information safely and securely.
Interoperability means data sharing between the health care member/patient, the health insurance company (insurer) and software applications on smart phones or computers. Beginning July 1, 2021, health care insurers must provide members with easy, standard and secured access to their health information from third-party apps.
Health care insurance providers store member information on computers. Health information must be easily accessible as patients move around from one health care provider to another.
Significance of Interoperability:
- Adheres to Center of Medicare and Medicaid (CMS) Mandate
- Insured member has easy access to their health information while ensuring security standards
- Caregiver can access patient information; parents can access dependent health information
Frequently Asked Questions
What is Interoperability?
An easy, secure way to exchange, access and integrate health information (Electronic Health Record (EHR)/Personal Health Record(PHR) and/or encounters) across systems. Access may be within any health system. App accesses the insurer’s system to get health information.
Why Interoperability?
Interoperability ensures that your health care insurer is compliant with federal government guidelines. Members get easy, secure access to health information. By sharing information with providers and using it for tracking personal health, members receive quality health care services and outcomes.
How to access Health Information?
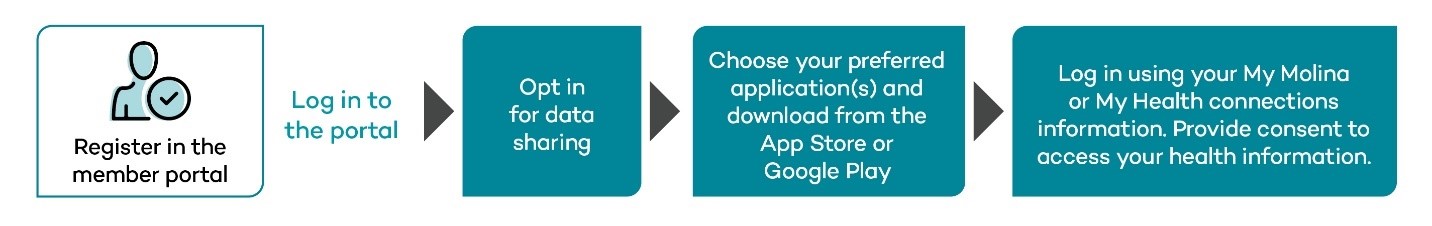
Follow the steps below to access your health information:
- Register on My Molina or My Health Connections member portal as applicable. Skip this step if you’ve already registered.
- Opt in for data sharing under Account Settings >> Manage Data-Sharing applications.
- Choose your preferred application(s) from the list of approved applications and download from the App Store or Google Play.
- Log in using your My Molina or My Health connections information. Provide consent to access your health information.
- As per CMS guidelines, the consent provided in your preferred applications(s) will be valid only for 90 days and you have to provide/renew consent for every 90 days.
Note: It may take up to 24 hours to see your health information after you’ve registered in the member portal and opted in to third-party applications.
What are all the third-party application Member can use?
What health information can members access?
Members have access to:
- Claims submitted by your provider
- Lab and diagnostic reports
- Medication data
- Provider Online Directory
- Prior authorization requests
Is the data current?
Per the CMS guidelines, members can access the latest health data 24 hours a day.
How much health history can members access?
Per CMS guidelines, members can access data from 2016.
How do I stop the application from accessing my health information?
Log in to My Molina or My Health Connections member portal. Navigate to PCE tab and revoke consent. Once consent is revoked, health information is no longer accessible on the app.
Can I access my child’s Health information?
Yes. Parent(s) can access children’s Health Information.
Can I delegate someone to receive access to my health information?
Yes. You must provide Power of Attorney (POA) to your Personal Representative (PR). Follow these steps:
- Call Member Services to provide PR/POA designation or submit the PR/POA form.
- Receive acknowledgment that PR/POA has been processed successfully.
- PR/POA to register on “My Health Connections” and create login credentials, PR/POA can call Member service for any assistance required.
- PR/POA can choose the preferred application and use “My Health Connections” Portal credentials to access member information.
- Once the PR/POA is assigned, care giver will have access to member portal on Member’s behalf and to comply with regulations, member will not have access to Member Portal.
As a Personal Representative (PR) or Power of Attorney (POA) how can I access Member’s Health information using any third party application?
As a PR/POA, Please follow below steps to access Member Health Information
- Register on “My Health Connections” portal. Skip this step if you’ve already registered.
- Opt-in for Interoperability in “My Health Connections” Portal.
- Choose your preferred application(s) from the list of approved applications and download from the App Store or Google Play or similar sources.
- Log-in to the Preferred applications(s) using your “My Health connections credential ”. Provide consent to access Member health information.
- As per CMS guidelines, the consent provided in your preferred application(s) will be valid only for 90 days and PR/POA must provide/renew the consent for every 90 days.
- In case PR/POA has been assigned as care giver for more than one member, you can use the same credentials to access all the member health information.
Please call (800) 642-4230 for more information and assistance.
Health plan data sharing
You can ask us to send your health information to another health plan. This is called health plan data sharing. Once you give us the okay, we will send your health information to the other health plan. The other health plan will then store your health information in their system. You should be able to request that they pass it on to any future health plan. This lets you take your health information with you from one health plan to another.
Who can make the health plan data sharing request?
A current or former member of ours or their authorized personal representative.
Can I have my child’s health information sent to another health plan?
Yes. Parents can submit the health plan data sharing request for their dependent minor children.
How do I request health plan data sharing with Molina Healthcare?
You can submit your request to us in one of these ways:
- Use your My Molina or MyHealth Connections portals:
- Login using your Molina user ID and password.
- Look for "Send My Health Information" option under Account Settings.
- Click on the link to access the health plan data sharing request form.
- Fill in the required information and submit the form.
- If you cannot use your member portal:
- Call our Molina Enterprise Service Desk at (800) 642-4230 choose option 6.
- Ask for a health plan data sharing request.
- Our agent will ask you questions and start the request.
- Our agent will fill in the form and submit the request on your behalf.
It’s as simple as that! We will tell you once the data is shared with the health plan you requested.
Please make sure you only request that data be sent to health plans that have a legitimate need for your health information. Once your request is received, we will send your heath data to the health plan requested.
What information will be shared with the other health plan?
We share all of your protected health information (“PHI”) that is stored by us from January 1, 2016. We do not share claims, encounter or administrative data.
The PHI that we share with the other health plan may contain sensitive health information that is subject to protections under federal and/or state privacy laws. Any use or further disclosure of such sensitive health information by the other health plan is subject to such privacy laws, as applicable.
Things to be aware of with health plan data sharing
- Beware of scammers. They may want to steal your health information.
- Share your data only with health plans you have active coverage with or that have a legitimate need for your health information. This helps you avoid sharing information with scammers.
- Check to make sure the health plan you intend to share your information with is known and trusted. Visit their public websites or contact them through customer service or official email.
To learn more about how to protect yourself from health insurance scams, please visit Spot Health Insurance Scams
When will my data sharing request be processed?
Once your request is submitted, we’ll process your request as quickly as possible. In some cases, it may take up to 30 business days.
How will I know the status of my data sharing request?
You can call our Enterprise Service Desk at (800) 642-4230 to check the status. You will get an email from us once your data has been sent to the health plan you requested.
In what cases can my data sharing request be denied?
We may deny your request if one of these things occurs:
- We cannot identify the health plan you requested.
- The other plan cannot accept your data from us.
We will contact you if this happens.
Are there any limits on the number of times a data sharing request can be made?
No. There are no limits on the number of times that you can submit the health plan data sharing request. We may not be able to process additional requests right away for the same member and health plan within the next 30 days of making the initial request.
Can I cancel a data sharing request?
No. Once you submit the request to us, you cannot cancel it.
Can Molina receive my health information from another health plan?
Yes. Molina can get your health information from your current or prior health plan.
How can I have my health information from my other health plans sent to Molina?
Please reach out to your other health plans and follow their directions to start the data sharing with Molina.
What will Molina do with my health information received from another health plan?
Molina will store the health information received from the other health plan along with your existing health information. When you ask us to send your health information to another health plan, we will share both the information received from your other health plans and your Molina health information.
Health plan data sharing: Instructions for other health plans
If you want to send a member(s) health information to Molina, call us at (800) 642-4230 and choose option 6 to reach our Molina Enterprise Service Desk. An agent will help you start an inbound health plan data exchange request.
Once your data sharing request is registered with us, our Interop Application Maintenance and Support team will reach you within 5 business days. We will discuss the process and details needed to receive the member data from you.
Find helpful resources, plan materials, payment information and more.